Why back pain belongs in the endometriosis conversation
Endometriosis is often framed as a “pelvic” problem. But many people with endometriosis also report low-back, sacral, hip, or buttock pain—sometimes in sync with the menstrual cycle, sometimes persistent between periods. That’s not incidental. Endometriosis is an inflammatory condition that can sensitize nearby tissues and nerves, affect posture and muscle tone, and—more rarely—irritate or entrap lumbosacral nerves (e.g., the sciatic nerve). Contemporary guidelines recommend a broad, person-centred approach that addresses gynecologic, musculoskeletal, and psychosocial drivers of pain. PMC+1
How endometriosis can cause (or worsen) back pain
1) Local inflammation that “turns up the volume” on pain
Endometriosis lesions release inflammatory mediators (e.g., prostaglandins, cytokines). Those chemicals can sensitize nociceptors (pain-sensing nerve endings) around the uterus, uterosacral ligaments, pelvic floor, and sacrum. The result can be aching in the low back or tailbone region, often with a cyclical pattern around menses. The 2022 ESHRE guideline (European Society of Human Reproduction and Embryology) emphasizes the heterogeneity of pain presentations and the need to consider extra-pelvic symptom referral. PMC
2) Deep infiltrating endometriosis (DIE) and the “muscle–fascia” link
When lesions infiltrate deeper structures—commonly the uterosacral ligaments or tissue near the rectovaginal septum—local muscles and fascia may guard in response. Over time that can create myofascial trigger points in hip rotators (piriformis), iliopsoas, and paraspinals; these can refer pain into the sacrum or lumbar region and flare with sitting or prolonged postures. Reviews published in 2024 highlight the importance of multimodal care for endometriosis-related pain, including attention to musculoskeletal contributors. ScienceDirect
3) Nerve involvement: when sciatica is cyclical
A smaller subset experience nerve entrapment or irritation (e.g., at the sciatic notch), producing “catamenial sciatica” (leg pain that worsens cyclically). MRI is the imaging modality of choice, and multidisciplinary management (gynecology, radiology, neurology/neurosurgery) is often required; in select cases, surgery can decompress the nerve and relieve symptoms. PubMed+1
4) Central sensitization and nociplastic pain
Chronic pain can “rewire” the central nervous system so that ordinary signals are felt as painful—a phenomenon called central sensitization (one mechanism of so-called nociplastic pain). In endometriosis, pain can be a mix of nociceptive (from tissue injury/inflammation), neuropathic (from nerve injury/irritation), and nociplastic (altered processing). A 2024 scoping review synthesizes tools and concepts for identifying central sensitization in endometriosis and underscores why education, graded activity, and psychological therapies can help. MDPI+1
5) The pelvic floor as a key hub
Pelvic pain, guarding, and stress can leave the pelvic floor over-active (hypertonic) or poorly coordinated. That can amplify low-back and sacroiliac pain and make sitting or bowel/bladder function uncomfortable. Emerging evidence suggests pelvic-floor-focused physiotherapy can reduce pain and improve function in people with endometriosis and chronic pelvic pain. ScienceDirect+1
Getting the right diagnosis (and ruling out red flags)
What to expect in evaluation
-
Focused history and exam: Map pain timing (cyclical vs. persistent), distribution (low back, sacrum, buttock, leg), aggravators (sitting, menses), pelvic floor tone, and any neurologic symptoms.
-
Imaging: Pelvic ultrasound is often first-line. MRI is indicated when deep infiltrating disease, bowel/urinary tract involvement, or suspected nerve entrapment is on the table. If sciatica is cyclical, MRI with attention to the sciatic notch/lumbosacral plexus is recommended. PMC+1
-
Differentials to consider: Discogenic low-back pain, facet or sacroiliac joint pain, hip pathology, myofascial pain, and combined patterns are common and can co-exist with endometriosis.
Red-flag symptoms—seek urgent care
-
New or progressive leg weakness, foot drop, or numbness spreading in a nerve distribution
-
Bladder or bowel dysfunction, saddle anesthesia
-
Fever, unexplained weight loss, or severe night pain
These warrant prompt medical assessment regardless of the suspected pain driver. (Red-flag constructs align with international back-pain guidance.) NCBI
Treatment in 2025: what best evidence supports
There isn’t a single “silver bullet.” The strongest care plans are multimodal and person-centred, combining gynecologic options (hormonal or surgical) with rehabilitation and psychosocial support.
-
Gynecologic options: Hormonal therapies (e.g., progestins, combined oral contraceptives, GnRH analogues/antagonists with add-back) can suppress lesion activity and reduce inflammatory pain; selection depends on symptoms, side-effect profile, comorbidities, and fertility goals. Surgery (often laparoscopic excision) is considered for deep infiltrating disease, organ or nerve involvement, or refractory symptoms—ideally in experienced, multidisciplinary centres. PMC+1
-
Back-pain principles: The WHO’s 2023 guideline for chronic primary low-back pain emphasizes non-surgical care—education, exercise/physical activity, certain manual therapies, and psychological approaches—while discouraging routine opioid use or passive modalities without active components. These principles translate well when nociplastic mechanisms are present alongside endometriosis. Weltgesundheitsorganisation+1
Small, doable steps that add up
Below are practical, low-risk self-care strategies you can start now—to complement medical care, not replace it.
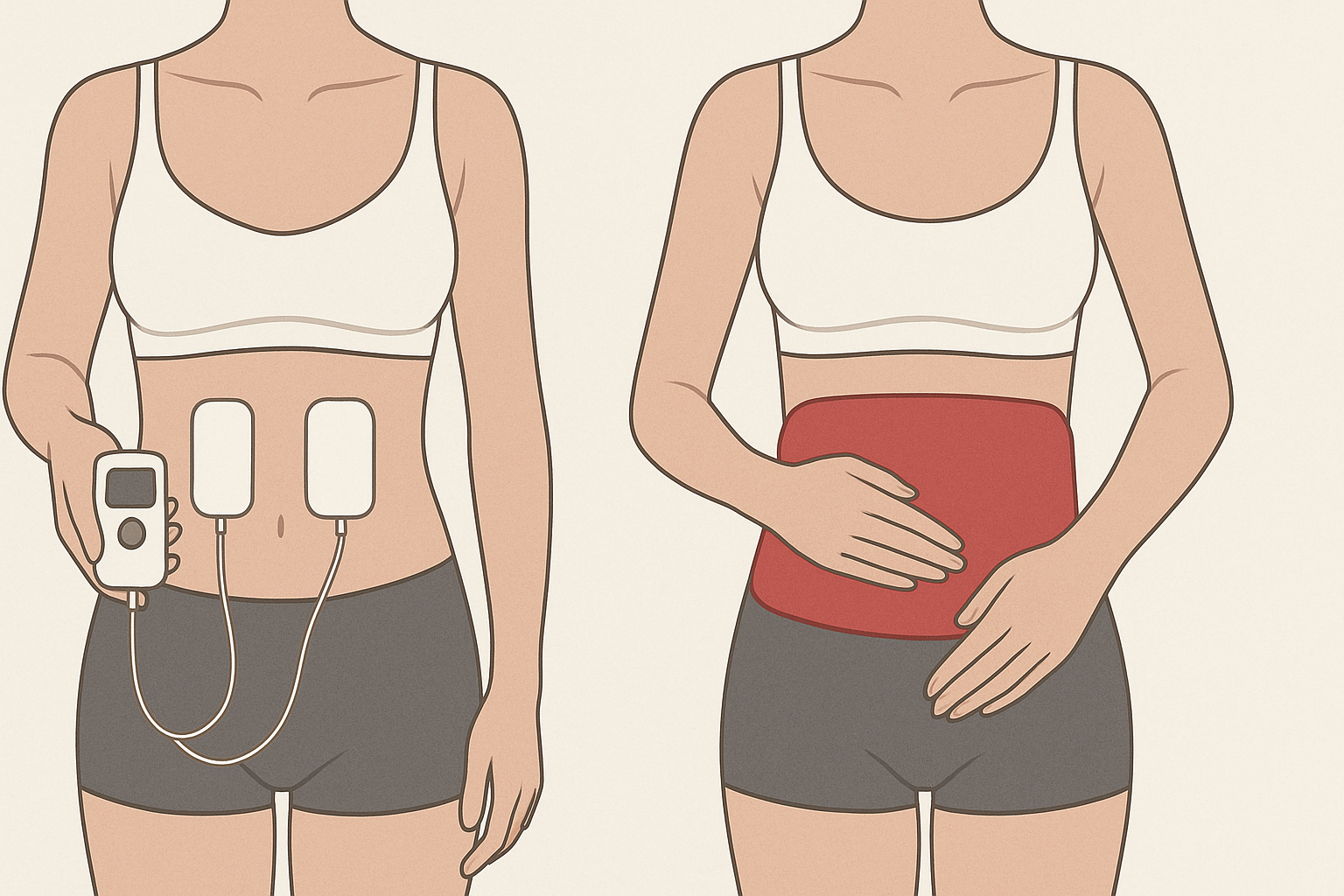
A) Soothing warmth: simple, safe, and often effective
Why it helps: Superficial heat improves blood flow, reduces muscle tone, and can dampen pain signaling. Reviews show continuous, low-level heat can provide short-term relief for nonspecific low-back pain and improve flexibility; many with endometriosis find warmth helpful for abdominal and low-back cramps. PMC+1
How to use it well
-
Apply a warm pack or heat wrap to the lower abdomen and/or low back for 20–30 minutes.
-
Combine heat with slow breathing (see below) to double down on nervous-system calm.
-
Safety: avoid sleeping with an active heating pad and protect skin if sensitivity is reduced. PMC
B) Sitting without the strain: movement beats “perfect posture”
Rather than chasing one “ideal” posture, aim for variety and breaks. Evidence suggests there’s no single posture that prevents back pain; it’s the long, static holds that tend to aggravate symptoms. Short, regular active breaks reduce back overload in prolonged sitting. JOSPT+1
Practical setup (rules of thumb)
-
Feet on the floor, hips and knees roughly 90°, forearms supported, shoulders relaxed.
-
Monitor at or just below eye level; screen at arm’s length.
-
Set a timer for 30–45-minute micropauses to stand, walk, or do two gentle mobility moves. Arbeitsschutzbehörde+1
C) Ten gentle minutes a day (a mini routine)
Goal: keep tissues mobile, down-regulate sensitivity, and build confidence in moving—without provoking flares. Start small; consistency matters more than intensity.
-
Diaphragmatic breathing (2 minutes)
Place hands over lower ribs. Inhale 4 seconds, pause 2–4, exhale 6–8. This lengthened exhale can reflexively relax pelvic floor and paraspinals. -
Cat–cow (1–2 minutes)
Slow arcs through pain-free range to mobilize the lumbar spine. -
Pelvic tilts in supine (1–2 minutes)
Gently rock the pelvis to find neutral; stop before pain. -
Knee-to-chest, alternating (1–2 minutes)
Ease tension in glutes and paraspinals. -
Hip-flexor lunge stretch (30–45 seconds each side × 2)
Short holds, smooth breathing. -
One-minute walk (hallway, stairs, outside)
Finish with motion that feels safe.
Yoga and mindful movement have shown improvements in pain and quality of life for endometriosis in small studies and reviews; while larger trials are needed, these modalities are low-risk when adapted to symptoms. PubMed+1
D) Pelvic-floor aware care
If you notice pain with sitting, sex, bowel movements, or urinary symptoms, ask your clinician for a referral to a pelvic-health physiotherapist. Interventions may include gentle manual therapy, down-training (relaxation/biofeedback), coordination work, and individualized home practice. Evidence—while still growing—shows meaningful functional gains and pain reduction in endometriosis-associated chronic pelvic pain. ScienceDirect+1
E) Stress, the nervous system, and pain (and what you can do)
Stress doesn’t “cause” endometriosis, but it can turn up pain sensitivity and muscle tension and disturb sleep—fuel for flares. Psychological interventions including cognitive-behavioral therapy (CBT) and acceptance and commitment therapy (ACT) improve pain coping, quality of life, and mental-health outcomes in women with endometriosis and in chronic pain more broadly. Internet-delivered options are being tested and show promise. Frontiers+2PubMed+2
Try a 5-minute daily de-stress
-
Choose one: paced breathing (4-4-6), body scan, progressive muscle relaxation.
-
Keep it tiny and daily. Protect sleep with a consistent wind-down (see next).
F) Sleep is an analgesic habit
Poor sleep lowers pain thresholds. Protect it with regular bed/wake times, a 30-minute wind-down (dim light, screen-off, warmth), and breathing or a brief body scan in bed. (Healthy-sleep and education-first strategies align with WHO back-pain guidance.) Weltgesundheitsorganisation
When you need more: medical options and team-based care
Hormonal therapy
Progestin-only therapies, combined hormonal contraceptives, and GnRH analogues/antagonists (usually with add-back regimens) can reduce bleeding and pain by suppressing ectopic endometrial activity. Choice is individualized; revisit decisions over time as goals change (e.g., fertility vs. symptom control). PMC
Surgery
For deep infiltrating disease, bowel/urinary tract involvement, or nerve endometriosis, referral to a high-volume centre is prudent. Outcomes improve when experienced multidisciplinary teams plan imaging, resection, and (if indicated) nerve decompression together. PMC
Rehabilitation & psychological therapies
Exercise programs (graded and symptom-adapted), pelvic-health PT, education about pain mechanisms, and CBT/ACT form the backbone of conservative care and complement gynecologic treatment. WHO emphasizes these non-surgical strategies for chronic back pain in primary/community care settings. Weltgesundheitsorganisation
Your quick-start plan (5 steps)
-
Book a review with your clinician if back pain is escalating, radiates below the knee, or brings numbness/weakness. Ask when MRI is indicated—particularly if pain is cyclical sciatica. PMC
-
Add warmth (10–20 minutes) before activity or stretching; avoid falling asleep on a heating pad. PMC
-
Move, don’t freeze: set a 30–45-minute timer for sit-breaks; implement the 10-minute mini routine daily. MDPI
-
Get pelvic-floor-savvy: seek pelvic-health PT if sitting/sex/bowel or bladder symptoms accompany your back pain. ScienceDirect
-
Tend to your nervous system: 5 minutes of CBT/ACT-style skills daily (paced breathing, values-based action, thought reframing); consider guided programs if available. Frontiers+1
FAQs
“My back pain isn’t clearly cyclical—could it still be linked to endometriosis?”
Yes. Mixed pain mechanisms are common—local inflammation, myofascial guarding, and central sensitization can maintain pain between periods. That’s why movement, education, and nervous-system strategies help alongside gynecologic care. PMC
“Is there a perfect sitting posture?”
No single posture prevents back pain. Vary positions and take active breaks; it’s the prolonged stillness that’s most provocative. Keep your monitor at or slightly below eye height and your screen an arm’s length away to reduce neck/shoulder load. JOSPT+1
“Is heat therapy ‘evidence-based’ or just comfort care?”
It’s both. Continuous, low-level heat wraps demonstrate small-to-moderate short-term benefits in nonspecific low-back pain; many people with endometriosis also find heat eases cramps. Use it as a supportive tool, not your only tool. PMC+1
“Can yoga really help?”
Small clinical studies and reviews suggest yoga and mindful movement can reduce pelvic pain and improve quality of life. Choose gentle, symptom-adapted sessions and avoid pushing into pain. PubMed
“What about medications for back pain?”
Short courses of NSAIDs may help some flare-ups. Routine opioid use is discouraged in chronic back pain; discuss risks and alternatives with your clinician. Weltgesundheitsorganisation
You’re not alone
If you live with endometriosis and back pain, you’re navigating a real, multifactorial pain condition—not “just period pain.” Many find that small, consistent steps—heat, gentle movement, sit-breaks, pelvic-floor awareness, and nervous-system skills—create meaningful change over weeks and months. Pair those with a supportive clinical team and community, and progress becomes more likely and more sustainable.
Sources (accessed September 23, 2025)
Guidelines & Overviews
-
Becker CM, et al. ESHRE Guideline: Endometriosis (2022). European Society of Human Reproduction and Embryology. PMC+1
-
WHO. Guideline for Non-Surgical Management of Chronic Primary Low Back Pain (2023) + news release. Weltgesundheitsorganisation+1
Mechanisms & Pain Science
3) Gentles AJ, et al. Nociplastic Pain in Endometriosis: A Scoping Review (2024). J Clin Med. MDPI
4) Saunders PTK, et al. Endometriosis: Improvements and challenges in diagnosis and treatment (2024). PMC
Nerve Involvement (sciatic/plexus)
5) Bindra V, et al. Sciatic nerve endometriosis – The correct approach matters (2023). PubMed+1
6) Zamurovic M, et al. Isolated Deep Infiltrating Endometriosis of the Sciatic Nerve (2023). PMC
Pelvic-Health Physiotherapy
7) Mansfield C, et al. Impact of Pelvic Floor Physical Therapy on Function in Chronic Pelvic Pain with Surgically Proven Endometriosis (2022). ScienceDirect
8) Can G, et al. Physiotherapy for Endometriosis-Associated Pelvic Pain (2025). Pain Medicine (ahead of print/online first). PubMed+1
Heat Therapy
9) Freiwald J, et al. A Role for Superficial Heat Therapy in Low Back Pain (2021). Narrative review; open access. PMC
10) Cochrane. Superficial Heat or Cold for Low-Back Pain (updated summary). Cochrane
Ergonomics, Sitting, and Active Breaks
11) Slater D, et al. “‘Sit Up Straight’: Time to Re-evaluate” (2019). JOSPT. JOSPT
12) Sortino M, et al. Active Breaks Reduce Back Overload during Prolonged Sitting (2024). J Clin Med. MDPI
13) OSHA. Monitor placement guidance (accessed 2025). Arbeitsschutzbehörde
14) Mayo Clinic. Office ergonomics: Your how-to guide (2023). Mayo Clinic
Exercise, Yoga, Mind–Body
15) Gonçalves AV, et al. Yoga for Pain-Associated Endometriosis (2017). PubMed
16) Murfitt P, et al. Systematic Review: Yoga for Endometriosis/CPP (2024). physiotherapyjournal.com
Psychological Interventions (CBT/ACT, digital options)
17) del Pino-Sedeño T, et al. Effectiveness of Psychological Interventions in Endometriosis (2024). Front Psychol. Frontiers
18) Donatti L, et al. Efficacy of Cognitive Behavioral Therapy in women with endometriosis (2025). PubMed
19) Ye L, et al. Acceptance and Commitment Therapy for Chronic Pain: Systematic Review (2024). PLOS
20) Schubert K, et al. Protocol: Internet-based CBT to improve QoL in Endometriosis (2022). BioMed Central
Medical disclaimer: This article provides general information and is not a substitute for personalized medical advice. Seek urgent care for red-flag symptoms (new weakness, numbness, bladder/bowel changes) or if your pain rapidly worsens.